Introduction
Welcome to Part 3 of our series exploring the importance of iodine and its connection to thyroid health. If you’re new to this discussion, we recommend reading Part 1 and Part 2 first. These previous articles provide valuable context on the iodine deficiency epidemic and Dr. David Brownstein’s insights into optimizing thyroid function through proper iodine intake, testing, and integrative treatment approaches. With this background, you’ll be better equipped to follow along with Part 3 without difficulty.
In this third blog post exploring the vital role of iodine, we dive into Dr. Brownstein’s decades of research and clinical experience revealing how correcting iodine deficiency through a comprehensive holistic approach could be key to preventing and treating glandular cancers.
Are you ready to continue strengthening your arsenal of well-being and health strategies? Let’s dive in, then!
Persistent High Rates of Glandular Cancers
In our modern world, we are surrounded by environmental toxins that can disrupt our body’s delicate balance. One crucial nutrient that is often overlooked is iodine, a mineral vital for overall health. Pioneering holistic doctors like David Brownstein, M.D., have been shedding light on the potential link between iodine deficiency and the alarming rise of certain cancers, particularly those affecting the glandular system.
While the exact statistics may vary across different sources and time periods, the prevalence of glandular cancers, such as breast, prostate, and thyroid cancers, is undoubtedly a pressing concern. Dr. Brownstein has highlighted this issue, stating, “As I have stated in my newsletters and books, I believe that iodine deficiency could be responsible for why one in seven U.S. women are suffering with breast cancer.”
Bear in mind that Dr. Brownstein’s claims regarding the prevalence rates were made some years back, showing small discrepancies with the most recent nationwide statistics.
According to the latest data from the American Cancer Society and National Cancer Institute, the burden of glandular cancers like breast and prostate cancer remains significant:
- Breast cancer affects approximately 1 in 8 women in the United States during their lifetime.
- Prostate cancer affects approximately 1 in 8 men in the United States during their lifetime.
Visualizing Cancer Trends
To provide a visual representation of these trends, let’s examine the following graph:
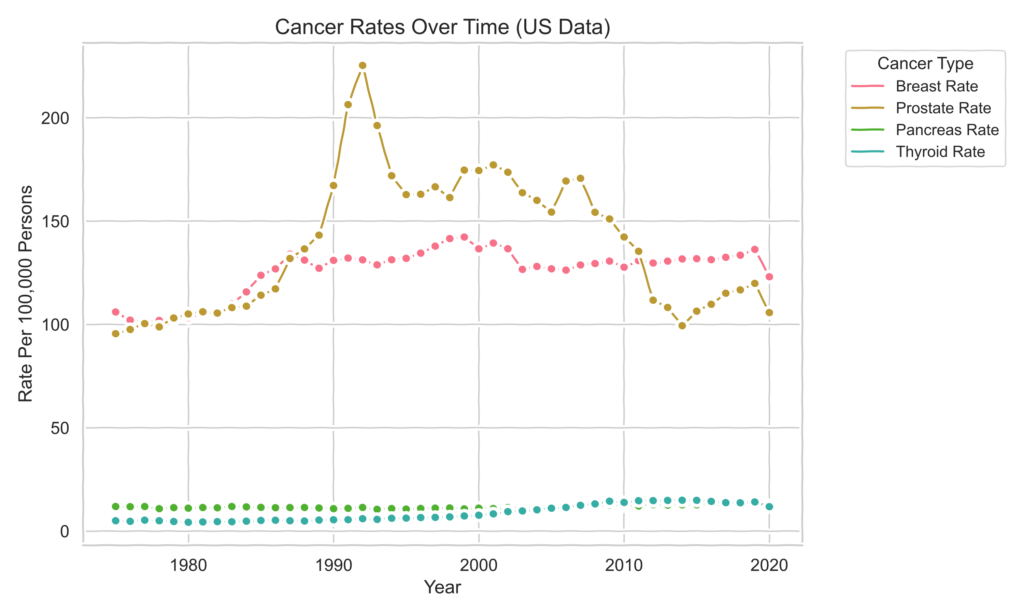
The graph shows the rates of different types of cancer over time in the United States. The prostate cancer rate increased from 1980 to 1992, then declined sharply from 2007 to 2014, likely due to changes in screening recommendations, and increased again until 2020. The breast cancer rate has been increasing steadily since 1980. The pancreas cancer rate has been increasing slightly since 1980. The thyroid cancer rate has been increasing rapidly since 1980. The 2020 data is included in the graph, but ignored for any data analysis as the lockdown during the pandemic may have affected the accuracy of the data, not providing a fair representation of the trends.
The overall trends in cancer rates are as follows:
- Prostate cancer: increasing
- Breast cancer: increasing
- Pancreas cancer: increasing slightly
- Thyroid cancer: increasing rapidly
Overall, this graph illustrates the concerning prevalence of breast and prostate cancers, two of the most common glandular cancers affecting women and men, respectively.
Normalizing Cancer Data for Better Visualization
A separate graph with normalized data will be introduced to better visualize the trends.

The normalized data shows that the thyroid cancer rate has increased dramatically over the last couple of years, although it seems to have stabilized since 2010. Breast cancer has also increased dramatically, and the pancreas cancer rate is increasing at a similar speed as breast cancer since 2004-2005. However, the most rapidly increasing is the thyroid cancer rate.
While there could be various factors contributing to these trends, such as early detection, screening methods, false positives/negatives, etc., a thorough analysis would be required to properly explain the data. However, delving into such an in-depth examination is beyond the scope of this blog article and would likely require a separate dedicated piece.
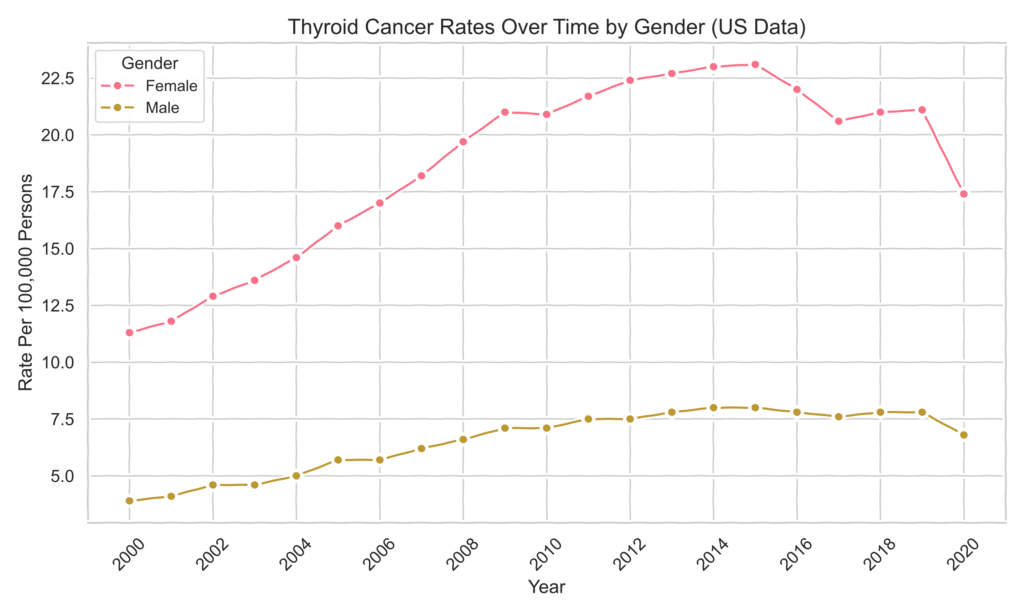
Thyroid Cancer: A Rapid Rise, Especially in Women
It is also important to note that this data does not distinguish between female and male. In the next graph, we will see the thyroid trend separate by sex, where we will see most of the rapid increase of thyroid cancer cases is associated with females.
Estimated New Cancer Cases for 2024
To provide further context from official data sources, let’s examine the estimated new cancer cases for 2024:

For females, the highest number of new cases is projected to be breast cancer at 310,720 cases. This is significantly higher than the next highest cancer, which is lung & bronchus cancer at 118,270 cases. Other major contributors include colorectum (71,270), uterine corpus (67,880), and colon (52,380) cancers.
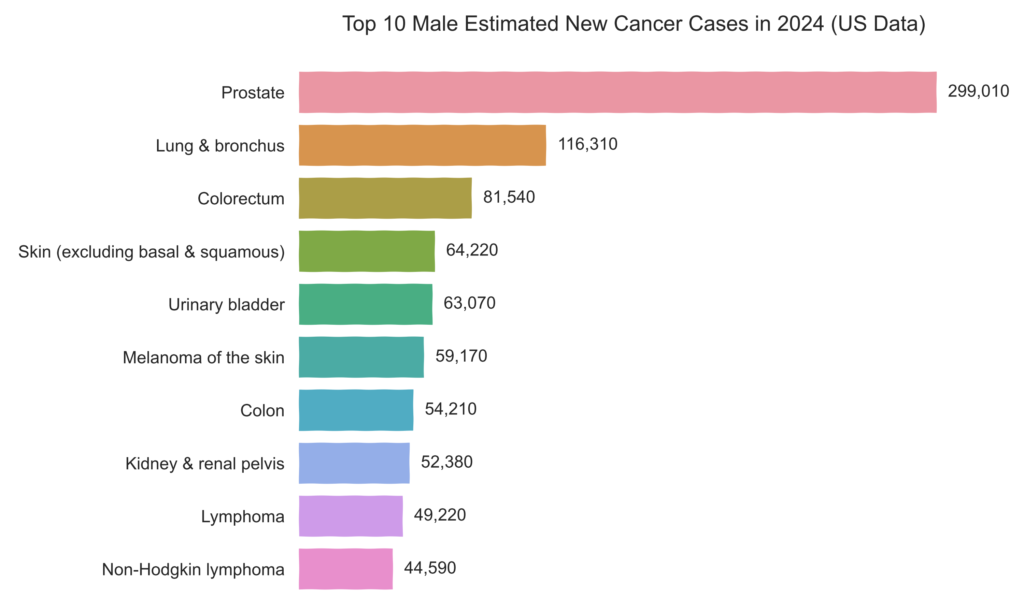
On the other hand, for males, the top estimated new cancer cases in 2024 are prostate cancer at a staggering 299,010 cases. This number is markedly higher than the second highest, which is lung & bronchus cancer at 116,310 cases. Colorectum cancer (81,540 cases) is also a significant contributor for males.
These graphs, based on data from official sources, illustrate the continued prevalence and significance of breast and prostate cancers among the estimated new cancer cases for 2024.
While statistics on cancer prevalence may vary across sources, the included graphs demonstrate the concerning rates of breast and prostate cancers that align with Dr. Brownstein’s observations from his extensive practice in holistic medicine. Notably, the graphs also reveal an alarmingly rapid increase in thyroid cancer cases during the last 40+ years, although with relatively fewer cases compared to breast and prostate cancers.
Dr. Brownstein’s holistic insights suggest exploring iodine deficiency’s role in glandular cancers, as he has seen potential iodine supplementation benefits. Let’s dive into what he has experienced and researched on this topic.
The Unique Role of Iodine in Glandular Tissue
Iodine is an essential mineral that actively concentrates in glandular tissues like the thyroid, breasts, prostate, and ovaries. Unlike other nutrients, it is transported into these glands against a concentration gradient using cellular energy via the “sodium-iodide symporter” (NIS) mechanism. This allows iodine levels inside the cells to be much higher than in the surrounding fluid. Why? Because one of iodine’s primary jobs is to maintain the normal architecture and structure of glandular tissue cells.
When iodine levels are insufficient in these tissues, Dr. Brownstein explains that a predictable series of events begins to unfold:
- Cysts start forming in the glandular tissue
- Over time, these cysts harden into nodules
- The nodules develop a precancerous “hyperplastic” appearance under a microscope
- If deficiency persists, the tissues can eventually progress to cancer
This concerning cascade from cyst to cancer caused by iodine deficiency has been demonstrated through test-tube studies, animal research, and extensive clinical observations in humans by Dr. Brownstein and others. “Remarkably, studies show that restoring adequate iodine levels can stop and even reverse this progression at any stage before full-blown cancer develops. So, my research – says Dr Brownstein – has clearly shown that iodine deficiency is one of the major causes of problems in these glands”.
Iodine’s Role in Hormone Production
Beyond just maintaining healthy glandular tissue architecture, iodine plays a critical role in the production of all hormones. It is essential for synthesizing thyroid hormones that regulate metabolism, but also the sex hormones estrogen, progesterone, and testosterone. Dr. Brownstein found that correcting iodine deficiency enabled many of his patients to reduce or discontinue supplemental bioidentical hormone therapy, as their bodies could better produce optimal hormone levels on their own with sufficient iodine.
Iodine’s Role in Reducing Breast Cancer Risk From Estrogen
Estrogen’s Complex Effects on Breast Cancer
It’s crucial to understand that estrogen’s role in breast cancer development is complex. While most breast cancers are ER-positive (approximately 75%), that is, breast cancer cells grow in response to estrogen, not all forms of estrogen have the same effects. This is where the misconception and fear surrounding the word “estrogen” often arise, leading to the belief that all estrogens are inherently bad and should be avoided.
Xenoestrogens: The Dangerous Endocrine Disruptors Increasing Risk
According to Dr. Brownstein, the real culprits contributing to accelerated rates of breast development, early puberty, and larger breast sizes seen in each newer generation of women are xenoestrogens – synthetic estrogen-mimicking chemicals ubiquitous in our modern environment. These compounds have a similar structure to estrogen, allowing them to bind to and saturate cellular estrogen receptors.
Unlike natural hormones that bind transiently to receptors, xenoestrogens “get stuck” and continuously stimulate these receptors in an unnatural way. This chronic excessive stimulation is what Dr. Brownstein believes fuels the increased risk of breast cancer and other estrogen-related issues.
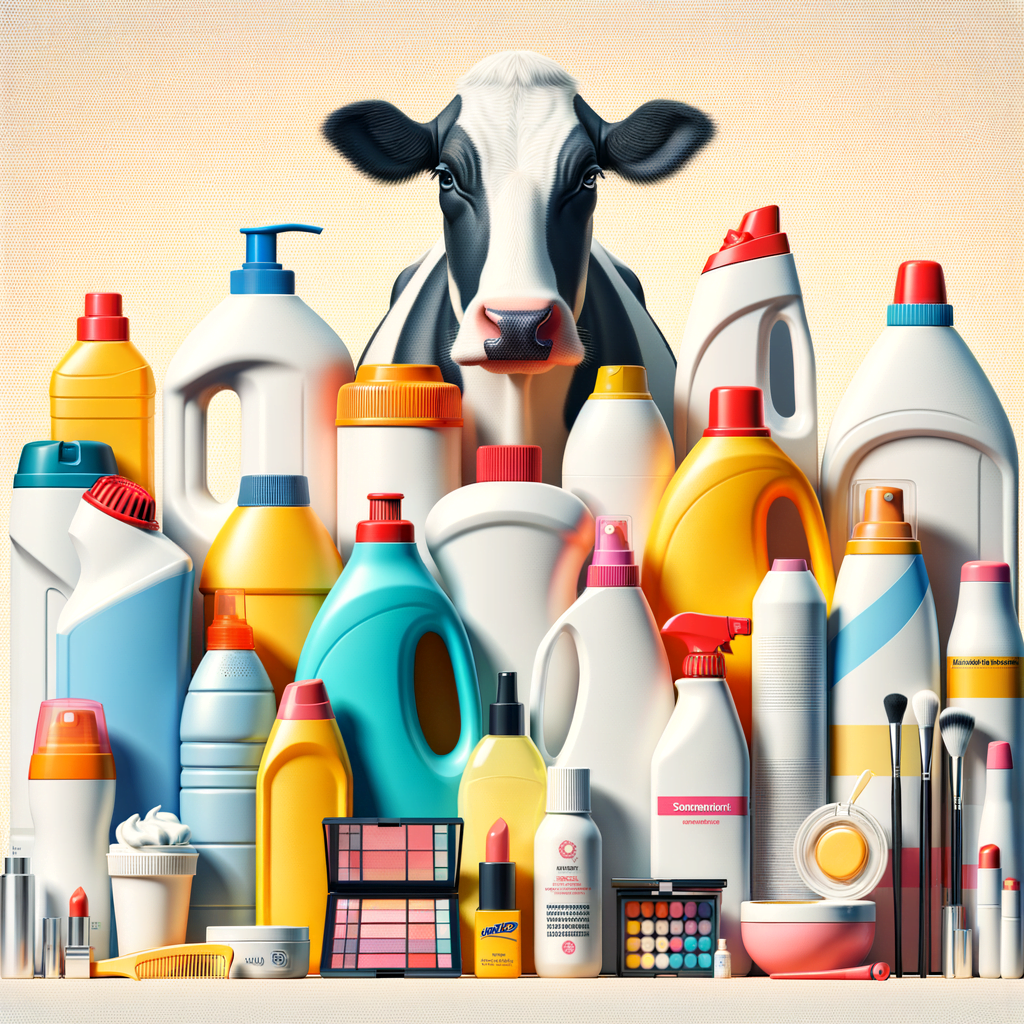
Top 10 Sources of Xenoestrogen Exposure to Avoid
Xenoestrogens are found in various products and sources, including:
- Commercial dairy and meat containing growth hormones
- Non-organic fruits and vegetables grown with pesticides, insecticides, herbicides, and fungicides
- Any products associated with plastics, including BPA in canned foods
- Commercial detergents and surfactants
- Chemicals in the water supply from detergents and surfactants
- Industrial chemicals such as dioxins, PCBs, and benzene-derived products
- Commercial sunscreens containing 4-MBC
- Antiperspirants made with metalloestrogens such as aluminum
- Commercial make-up and sundry products containing parabens
- Estrogenic drugs like birth control pills in the water supply
Iodine’s Critical Role in Detoxifying Xenoestrogens and Halides
Dr. Brownstein identifies two key factors driving widespread iodine deficiency: xenoestrogen compounds and toxic halide exposures.
As we have already mentioned in the previous two articles, the prevalence of halides like bromide and fluoride act as iodine displacers and impersonators, disrupting iodine’s crucial biological roles in glandular tissues. Pesticides, insecticides and non-organic foods contain high levels of these iodine-depleting halide contaminants.
Additionally, xenoestrogens – the ubiquitous synthetic estrogen-mimicking chemicals in our modern environment – contribute to an effective iodine deficiency state. These compounds can saturate and “get stuck” on cellular estrogen receptors, creating chronic excessive stimulation.
Adequate iodine appears to play a crucial role in metabolizing and detoxifying both xenoestrogens and halides more effectively. Iodine helps “unstick” stubborn xenoestrogens from receptor sites, while also displacing halides that mimicked and depleted iodine stores.
To counter the effects of both xenoestrogens and toxic halides, Dr. Brownstein emphasizes the need for:
- Gentle detox protocols to remove built-up halide and xenoestrogen burdens.
- Optimizing iodine levels through supplementation to replete deficits.
The Breast Cancer-Protective Benefits of Phytoestrogens
While xenoestrogens and higher levels of certain estrogens may contribute to breast cancer risk, it’s important to understand that not all estrogen-like compounds are harmful. Phytoestrogens, plant-derived compounds with estrogen-like properties, are often referred to as “gentle estrogens” or “anti-estrogens” due to their potential healing effects rather than carcinogenic effects.
As explained by Dr. Veronique Desaulniers in her book on breast cancer, there are two different types of estrogen receptors present on cells: estrogen receptor alpha (ER-α) and estrogen receptor beta (ER-β) sites. Natural estrogens and chemical xenoestrogens both seek out ER-α sites on cells. However, soy phytoestrogens have a much greater affinity for ER-β sites.
- Think of our cells as little houses, and the estrogen receptors (ER-α and ER-β) as different types of doors.
- Regular estrogens like to go through the ER-α doors, while soy estrogens (isoflavones) prefer the ER-β doors.
- When soy estrogens start going through the ER-β doors, the cells start favoring the instructions (genes) to make more ER-β doors and fewer ER-α doors.
- This way, there are fewer doors for the regular estrogens to go through, which can help reduce the risk of breast cancer.
It’s important to note that the beneficial effects of soy are associated with consuming whole, fermented soy products, such as organic miso paste, natto, tempeh, and pickled tofu, rather than isolated soy supplements. These are the recommendations from Dr. Veronique Desaulniers.

Long-Term Thyroid Medication Worsens Breast Cancer Risk
Two surprising studies found that women taking thyroid hormone medication long-term, for at least 15 years, had an almost 200% increase risk of developing breast cancer compared to women not on these medications. How could that be?
The answer became clear once he understood the role of iodine deficiency. When taking thyroid medications, the increased metabolic rate and energy demands triggered by the medication exacerbate any existing iodine deficiency in the body. Over years of compounded iodine deficit as metabolism is artificially revved up, this slowly disrupts the healthy architecture of glandular tissues like the breasts and likely promotes cancerous changes.
The sobering implication is that thyroid patients deficient in iodine may have been putting themselves at greater breast cancer risk by just taking thyroid medication alone. Combining iodine supplementation is likely crucial for safely optimizing thyroid health and preventing unintended consequences.
According to Dr. Brownstein’s experience, perhaps only around 1/3 of women taking thyroid hormone actually require it, while another 1/3 may need both thyroid hormone and iodine supplementation. The remaining 1/3 may simply need iodine alone to help rectify their thyroid levels. He recommends checking iodine levels first, and if supplementation is required, combining it with thyroid hormone for those who truly need the medication.
In his practice, this iodine-focused approach reduced the number of patients requiring thyroid medication from 3/4 to only 1/3. For those still needing medication, their dosage could often be cut in half when combined with iodine.
The Concerning Rise of Prostate Cancer in Young Men
While breast cancer has been the prime focus of iodine deficiency’s role, Dr. Brownstein has also witnessed alarming increases in prostate cancer in his practice – especially in younger male patients, an extremely rare occurrence just decades ago.
The mechanisms mirror breast disease – iodine maintains the prostate’s healthy glandular architecture, while deficiency allows cysts, nodules, and precancerous hyperplasia to take root over time. Incorporating iodine into holistic treatment plans has allowed Dr. Brownstein to stabilize cases of early-stage prostate cancer and dramatically slow prostate-specific antigen (PSA) rise, indicative of prostate cancer presence.
Stephanie’s Powerful Testimonial
Few stories illustrate the transformative impact of holistic iodine therapy better than that of Dr. Brownstein’s patient Stephanie. Diagnosed with thyroid cancer after giving birth, Stephanie was treated with radioactive iodine ablation and placed on long-term thyroid medication – a regimen that ultimately failed to resolve her progressive symptoms like fatigue, joint pain, and severe anxiety.
Disillusioned after one doctor flippantly told her to just “throw food at her kid in a highchair” during her radiation recovery, Stephanie finally found Dr. Brownstein years later. On his holistic program incorporating high-dose iodine, nutrients, and detox protocols, Stephanie’s lifelong improvement was dramatic:
“By the first 6-7 months I was maybe 75-80% better… It was like a light bulb went out of my brain. The joint pain I had just started to melt away. My energy went up… By that summer we were able to go to the Detroit zoo and walk the whole thing. I was just totally amazed because that would have laid me out flat for days before.”

With continued holistic treatment, Stephanie has remained cancer-free since 2009 and regained her vitality as a mom. The contrast between her previous fragmented care focused only on medication and Dr. Brownstein’s comprehensive approach aimed at addressing the root iodine deficiency could not be more striking.
Conclusion
And now, as we approach the end of our exploration, let’s reflect on what we’ve learned today from Dr. Brownstein’s decades of research and clinical experience.
Dr. Brownstein’s extensive work has shed light on the pivotal role optimizing iodine levels can play in preventing and treating glandular cancers like breast, prostate, and thyroid cancers. The powerful testimonial from his patient Stephanie exemplifies the transformative impact of this holistic, iodine-focused approach.
The key takeaways include:
- Proper iodine supplementation tailored to individual needs can help maintain the healthy architecture and structure of glandular tissues, preventing the progression from cysts to nodules to precancerous changes that iodine deficiency can fuel.
- Adequate iodine aids in detoxifying xenoestrogens (environmental estrogen-mimicking compounds) and halides like bromide and fluoride, which deplete iodine stores and disrupt hormone balance.
- For thyroid patients, combining iodine supplementation with medication may be crucial to prevent unintended consequences like increased breast cancer risk from long-term thyroid medication alone.
As you consider supplements or holistic approaches, remember to consult your healthcare provider first. Keep an open yet discerning mindset, building your knowledge wisely.
Let’s wrap up with a call to action!
Do not hesitate to share your insights, experiences, and thoughts in the comments below. This discussion space allows us to learn from each other’s journeys. Your perspective could provide an “aha” moment for fellow readers. Stay curious, stay healthy!
Resources
- Official Dr David Brownstein website: Dr Brownstein website
- Dr Brownstein ‘Overcoming Thyroid Disorders’s book’: Overcoming Thyroid Disorders
- Leading Cancer Cases and Deaths, All Races and Ethnicities, Male and Female, 2020: Cancer Statistics At a Glance
- Scientific research reports an increased trend of thyroid cancer incidence in the south of Spain: Thyroid Cancer Epidemiology in South Spain: a population-based time trend study
- Scientific research on differential incidence trends of conventional and follicular variant papillary thyroid cancer in the USA: Recent incidences and differential trends of thyroid cancer in the USA
- Scientific research on the study of thyroid cancer (TC) mortality in Ecuador during 1990-2016: Trends of Thyroid Cancer Mortality Rates in Ecuador
- Study showing iodine can slow the growth of breast cancer cells in the lab: Changes in Dietary Iodine Explains Increasing Incidence of Breast Cancer with Distant Involvement in Young Women
- Study reporting on the role of iodine in breast tissue growth and development, and the potential implications of iodine deficiency for breast cancer risk: Iodine and mammary cancer
- Study investigating the use of iodine replacement therapy for fibrocystic breast disease: Iodine replacement in fibrocystic disease of the breast
- Scientific research shows iodine may protect against breast cancer: The Extrathyronine Actions of Iodine as Antioxidant, Apoptotic, and Differentiation Factor in Various Tissues
- Scientific research suggests that iodine is an antioxidant and antiproliferative agent that may play a role in the prevention and treatment of breast cancer: Is iodine a gatekeeper of the integrity of the mammary gland?
- Blog post by the naturopath Amy LaRue about xenoestrogens: Xenoestrogens – What are they? How to avoid them